If you’ve experienced sudden jolts or a strange electric-like shock sensation in your head, you’re not alone. Known as “brain zaps,” these symptoms often appear when people stop or reduce certain medications, especially antidepressants.
They can be unsettling, and while they aren’t dangerous, they can make the process of adjusting or tapering off medications difficult.
In this guide, we’ll explore why brain zaps happen, what they feel like, and ways you can manage them to make the transition smoother.
Key Takeaways
- Brain zaps are common when stopping or reducing antidepressants.
- They feel like sudden, brief electric shocks in the head.
- Gradual tapering and some lifestyle changes may help reduce their severity.
What It Feels Like?
- Electric Shocks: Often described as a brief shock or buzzing inside the head.
- Visual and Auditory Disturbances: Some report flashes of light or hearing sounds, like a swoosh or pop.
- Vibrations: Some people liken it to a brief vibration or tingling in the head.
- Momentary Disorientation: Occasionally, they cause a sense of detachment or “brain skipping a beat.”
Main Causes

Brain zaps are thought to result from sudden neurotransmitter shifts, particularly with serotonin and norepinephrine, as the body adjusts to medication changes. Medications with shorter half-lives, like Zoloft or Paxil, can leave the body more quickly, potentially leading to more noticeable symptoms if not tapered gradually.
According to Psychiatrist.com, brain zaps often arise from abrupt changes in neurotransmitter levels, particularly serotonin, during the discontinuation of antidepressants.
Castle Craig highlights that the issue often stems from sudden neurotransmitter shifts, particularly serotonin, triggered by stopping medications like SSRIs. Shorter half-life drugs, such as venlafaxine, can exit the system rapidly, leading to abrupt serotonin drops and sensory disruptions. The role of GABA may also play a part, with reduced levels potentially adding to these sensations.
Common Triggers and Symptoms
Movements of the eyes or head frequently trigger these sensations. Studies suggest that individuals who have recently discontinued antidepressants experience the issue more intensely when they shift their gaze quickly or move their head side to side. These sudden sensations can be startling, leading to momentary dizziness or disorientation.
Aside from physical movement, factors like stress, sleep disruption, and fatigue are common triggers. A study published in The National Library of Medicine found that brain zaps often correlate with stress and fatigue levels in patients adjusting to medication changes, indicating a link between physical and mental stressors in the onset of brain zaps.
Key Symptoms
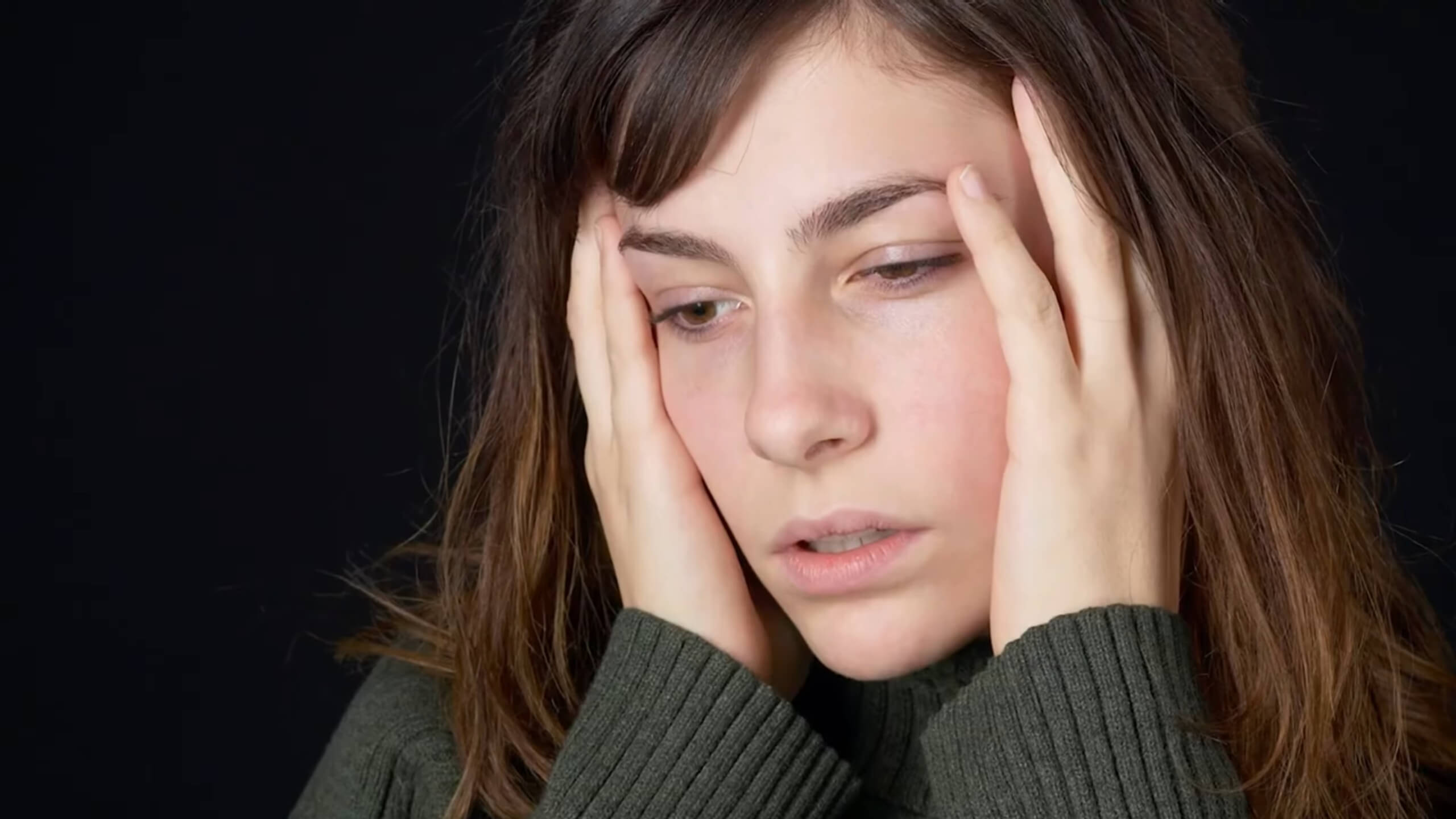
- Electric Shocks and Vibrations: A sudden jolt in the head, often felt as an electric shock or buzzing.
- Dizziness and Disorientation: Can cause brief, intense vertigo, leading to a feeling of light-headedness.
- Auditory and Visual Disturbances: Some people report hearing a “pop” or “swish” sound and seeing brief flashes of light when a brain zap occurs.
Also, read more about generational trauma and what can cause it.
Key Characteristics
- Electric Shocks: Most people report a shock-like sensation inside the head.
- Buzzing and Popping Sounds: Sudden auditory sensations often accompany brain zaps, which can create an additional feeling of disorientation.
- Momentary Loss of Focus: Brain zaps can cause brief lapses in concentration, leading to a sensation of mental “blinking.”
How to Deal With the Issue?

Dealing with it often involves gradual tapering and supportive strategies to help the body adjust to medication changes. The most effective way to reduce brain zaps is to avoid abrupt medication discontinuation, opting for a slow, controlled reduction over several weeks or even months.
This approach allows the brain to gradually adjust to lower neurotransmitter levels, reducing the chance of sudden disruptions.
Some people find relief through lifestyle adjustments and supplements. Omega-3 fatty acids, found in fish oil, are often recommended as they support brain health and may help buffer against some withdrawal effects.
Additionally, staying hydrated and maintaining a balanced diet can assist in reducing fatigue and stress, both of which are known to exacerbate brain zaps.
Practical Strategies to Minimize the Effects
- Follow a Gradual Tapering Schedule: Work with a healthcare provider to plan a tapering schedule suited to your needs.
- Incorporate Omega-3s: Adding omega-3-rich foods or supplements may support neural health during withdrawal.
- Practice Stress Management: Meditation, yoga, and breathing exercises can help lower stress, which might reduce the intensity of brain zaps.
- Avoid Caffeine and Alcohol: These can intensify symptoms for some people, so reducing intake can help ease discomfort.
- Stay Active: Regular physical activity helps stabilize mood and promotes better sleep, both of which can make the withdrawal process smoother.
When to Consult a Doctor
If brain zaps persist or worsen, or if they interfere significantly with daily life, consulting a healthcare provider can be essential. Brain zaps, while often temporary and manageable, can sometimes indicate the need for a more tailored withdrawal plan.
A healthcare provider can assess the severity of symptoms and adjust tapering methods or offer alternative options, such as switching to a longer-acting medication, which may reduce the frequency of zaps.
In some cases, intense brain zaps might accompany other symptoms like severe dizziness, nausea, or even heightened anxiety. If this occurs, it’s crucial to reach out to a professional, as these symptoms can sometimes mimic or mask a relapse of underlying conditions.
A provider might also recommend supportive therapies, such as counseling, to help with emotional adjustments during withdrawal.
Ways to Manage Antidepressant Withdrawal Symptoms

Managing antidepressant withdrawal requires strategies that directly address physical and mental discomfort. A gradual reduction plan under medical supervision is essential to reduce sudden changes in brain chemistry.
Practicing regular breathing techniques or grounding exercises can also lessen the impact of symptoms, particularly brain zaps, by calming the nervous system.
Quality sleep, regular hydration, and meals stabilize your body’s baseline, helping it better handle the absence of medication. Some people find that omega-3 supplements or B vitamins support nerve health, but always consult a professional before starting any supplement.
Tips to Consider
- Controlled Tapering: Avoid sudden stops. Gradual dose reduction helps prevent intense symptoms.
- Stay Hydrated and Eat Regularly: A steady routine can keep your body balanced and ready to handle changes.
- Relaxation Techniques: Breathing exercises or light activities can reduce stress, making symptoms easier to manage.
Could Changing Certain Habits Help?
Certain lifestyle adjustments can help manage symptoms during antidepressant withdrawal. Regular physical activity, such as walking or stretching, can improve circulation and reduce stress, which may help reduce the severity of brain zaps.
Additionally, cutting down on caffeine and alcohol may lower nervous system sensitivity, reducing symptoms like dizziness or jitteriness.
Sleep is a critical factor. Establishing a consistent bedtime and ensuring quality rest supports brain health and helps stabilize mood, which can alleviate some of the mental strain of withdrawal.
Staying hydrated and eating nutrient-dense foods also provide essential support, helping the body maintain balance and manage neurotransmitter shifts more smoothly.
Lifestyle Tips to Support Withdrawal

- Consistent Physical Activity: Low-impact exercise helps ease stress and promotes mood stability.
- Limit Caffeine and Alcohol: Reducing stimulants can lower nervous system sensitivity.
- Quality Sleep Routine: A regular sleep pattern provides essential support for mood and brain function.
- Balanced Nutrition: Nutrient-rich foods and hydration aid in maintaining energy and stability.
FAQs
How long do brain zaps usually last?
Brain zaps typically last from a few days to several weeks, depending on the individual and the medication being discontinued. Some people may experience them for longer, but gradual improvement is common over time.
Can brain zaps cause permanent damage?
No, brain zaps do not cause permanent brain damage. They are usually temporary sensations caused by changes in neurotransmitter levels and generally resolve as the body adapts to medication withdrawal.
Do brain zaps only happen with antidepressants?
While brain zaps are most common with antidepressant discontinuation, they can also happen with other medications that affect neurotransmitters, such as benzodiazepines or some sleep aids. Even occasional use of certain substances can trigger similar sensations in sensitive individuals.
Are brain zaps dangerous if they happen while driving?
Brain zaps are not dangerous in themselves, but if they cause dizziness or disorientation, it may be unsafe to drive. If you experience frequent or intense brain zaps, avoid driving until symptoms are more manageable.
Can anxiety trigger brain zaps?
Yes, anxiety can sometimes increase the intensity or frequency of brain zaps, as stress affects neurotransmitter balance. Relaxation techniques like deep breathing or mindfulness may help reduce their impact during anxious moments.
Can I prevent brain zaps if I go off medication slowly?
A slow tapering process significantly reduces the likelihood and severity of brain zaps but may not eliminate them entirely. Consult a healthcare provider for a gradual tapering schedule to minimize withdrawal symptoms effectively.
Wrapping Up
Brain zaps can be a tough part of coming off antidepressants, but they’re usually temporary. Reducing meds slowly and giving your body time to adjust is key to managing the effects.
Simple changes like focusing on good sleep, balanced meals, staying hydrated, and finding ways to relax can make a big difference. Symptoms vary, so if brain zaps disrupt your day, talk to a doctor for options that fit your situation.
They’re uncomfortable but not harmful, and with the right approach, they usually pass in time.
Sources
- Verywell Mind – https://www.verywellmind.com/brain-shivers-as-effexor-withdrawal-symptom
- Health.com – https://www.health.com/condition/depression/brain-zaps
- Psychiatrist.com – https://www.psychiatrist.com/news/3-key-studies-on-brain-zaps-in-antidepressant-withdrawal/
- Castle Craig – https://www.castlecraig.co.uk